As we age, our bodies undergo a series of changes that often manifest in the form of orthopaedic issues. From what I have seen in my career as an orthopaedic doctor, the age of 40 is a common milestone when some of these problems become more pronounced. Understanding what to expect can help individuals remain proactive about their health and seek appropriate medical care when necessary. Read on as Dr Syed Imran, Consultant Orthopaedic, Arthroscopy and Joint Replacement Surgeon shares five orthopaedic issues that are common in people above 40.
Orthopaedic Problems After Age 40
Here are five common orthopaedic problems one might experience after hitting the big 40:
Osteoarthritis (OA)
This is the most common type of arthritis, caused due to wearing down of cartilage that provides cushioning to the bones. This is common in hands, knees, spine and hip.
What Causes Osteoarthritis?
According to Dr Imran, the exact cause of OA is multifaceted. While age is a significant factor, other contributors include:
- Genetics: Some people inherit genes that make them more susceptible to OA.
- Joint injuries: Past injuries, such as torn cartilage or dislocated joints, can increase the risk of developing OA in the future.
- Obesity: Carrying extra weight puts additional stress on weight-bearing joints, particularly the knees, hips, and spine, increasing the risk of wear and tear.
Managing OA
While there's no cure for OA, a combination of strategies can help manage symptoms of osteoarthritis:
- Medications: Over-the-counter pain relievers and anti-inflammatories can help alleviate pain.
- Physical therapy: A physical therapist can devise exercises to strengthen the muscles around your joint, increasing its stability and reducing pain.
- Lifestyle modifications: Maintaining a healthy weight and staying active can help reduce symptoms and prevent the progression of OA.
Osteoporosis
Dr Imran shares, "As we age, bone density decreases, making bones more fragile and prone to fractures. Osteoporosis particularly affects postmenopausal women, although men can also develop it. Regular checkup after 40, a calcium-rich diet, weight-bearing exercises, and certain medications can help manage and prevent osteoporosis."
What Causes Osteoporosis:
- Hormonal Changes: Reduction in estrogen levels during menopause in women and a decrease in testosterone in men can lead to osteoporosis.
- Calcium and Vitamin D Deficiency: Insufficient intake or poor absorption of these essential bone nutrients can weaken bone density.
- Certain Medications: Long-term use of corticosteroids or some antiseizure medications can reduce bone density.
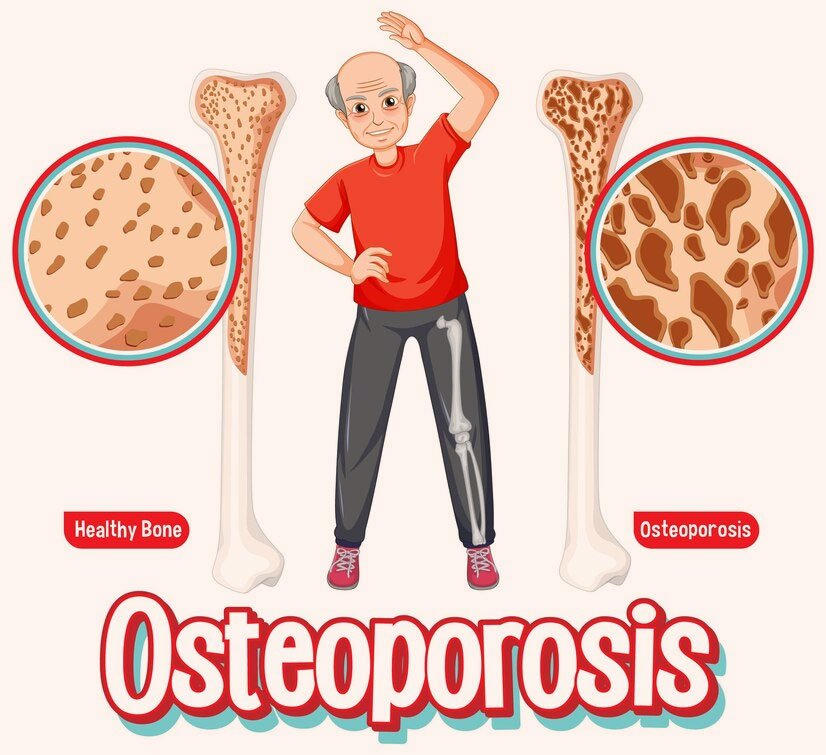
Managing Osteoporosis:
- Dietary Changes: Increase intake of calcium and vitamin D through foods like dairy, green leafy vegetables, and fish.
- Supplements: Consider taking calcium and vitamin D supplements if dietary intake is insufficient.
- Exercise: Engage in regular weight-bearing exercises like walking, dancing, or resistance training to strengthen bones.
Rotator Cuff Tears
"With age, rotator cuff tendons can degenerate or become damaged, often due to repetitive overhead motions. Symptoms include pain at rest and at night, weakness when lifting or rotating the arm, and a crackling sensation when moving the shoulder," explains Dr Imran.
What Causes Rotator Cuff Tears:
- Ageing: Natural wear and tear over the years can weaken and degenerate tendons, making them more susceptible.
- Repetitive motion: Overhead activities (like painting, lifting, or playing certain sports) can strain the rotator cuff.
- Acute injury: A sudden force or trauma, like a fall on an outstretched arm or lifting something heavy abruptly.
Managing Rotator Cuff Tears:
- Rest: Avoiding activities that worsen the pain or strain the shoulder.
- Cold compress: Applying ice packs can reduce inflammation and pain.
- Physical therapy: Strengthening exercises and stretches can restore function and alleviate pain.
Degenerative Disc Disease

Over time, the discs between the vertebrae in our spine can break down, leading to degenerative disc disease. This condition can cause chronic neck or lower back pain. Activities that were once easy, such as bending or twisting, may become painful. Although it's part of the natural ageing process, certain factors like obesity, smoking, or injury can exacerbate the condition.
What Causes Degenerative Disc Disease:
- Natural Ageing Process: Over time, the discs in our spine lose hydration and elasticity, leading to decreased ability to act as shock absorbers.
- Wear and Tear: Everyday movements and activities can cause wear on the discs.
- Injuries: Trauma to the spine, such as from a fall or car accident, can start or accelerate the degeneration of discs.
Managing Degenerative Disc Disease:
- Physical Therapy: A well-structured physical therapy program can help strengthen back muscles and improve flexibility.
- Exercise: Low-impact activities such as walking, swimming, or cycling can reduce pain and improve back health.
Tendinitis and Bursitis
Both conditions are associated with inflammation. Tendinitis affects the tendons, which are cords that attach muscle to bone, while bursitis concerns the bursae, small, fluid-filled sacs that cushion bones, tendons, and muscles. Common areas affected include the shoulder, elbow, hip, and knee. Overuse, injury, and age-related wear and tear are common culprits.
What Causes Tendinitis and Bursitis:
- Overuse: Repetitive motions or activities can strain the tendons or irritate the bursae.
- Injury: Direct trauma or sudden, forceful movements can lead to inflammation of the tendon or bursa.
- Age: As we get older, tendons lose their elasticity and bursae can become more prone to inflammation.
Managing Tendinitis and Bursitis:
- Rest: Give the affected area a break to reduce inflammation and prevent further injury.
- Ice: Use ice packs on the affected area to reduce pain and swelling.
- Compression: Use bandages or braces to support the affected area.
Final Word
Reaching our 40s doesn’t mean we're destined to experience these orthopaedic issues, but being aware of them allows us to take preventative measures and seek timely interventions. Regular check-ups, a balanced diet, proper exercise, and an awareness of our body's signals can help mitigate the effects of these conditions and ensure we remain active and pain-free for years to come.